Workers and local communities are not to blame; responsibility lies with employers, regulatory agencies and government
Summary
It seems nearly every day there is another outbreak of Covid-19 in Britain’s factories, in the food processing industry, in the garment industry and elsewhere. It is increasingly clear that working conditions in the factories are largely responsible for the outbreaks, in particular by means of airborne spread of Covid-19. In contrast spread between workers outside the factory and in local communities plays only a small part. The timing, circumstances and pattern of the outbreaks, points to them being typical “super-spreader events”, caused by airborne spread of the virus within the same enclosed indoor space of the factory, from one or two infected individuals to large numbers of other workers. The actions of workers themselves play only a minor role in these outbreaks; the task before us is to urgently take measures to address the airborne route of spread, not only in factories but in all workplaces and schools, if we are to reduce outbreaks.
The spread of Covid-19 in indoor spaces is extremely difficult to prevent entirely. There is in reality no such thing as a “Covid-safe” workplace or school, unless transmission in the community is eliminated. The rate of community transmission will determine what happens in our workplaces and schools and a national “Zero Covid” strategy is therefore essential. We can make indoor spaces safer by hygiene measures, distancing, wearing masks and proper ventilation. We should be spending as much time talking about ventilation as we do the other measures. The Health and Safety Executive, the Food Standards Authority and other regulatory authorities have a crucial role in ensuring this is done properly; so far we have heard very little from them during the whole of the Covid-19 pandemic.
This briefing discusses airborne spread and the lessons we need to learn from super-spreading events which have occurred here and in other countries. This is all the more urgent as we head into autumn and winter when we all move indoors to a much greater extent.
Contents
- Airborne spread of Covid-19
- Greencore outbreak
- Tönnies meat packing plant study
- Preventive measures taken by Tönnies and lessons learned
- Growing evidence and consensus around aerosol spread
- Workers and local communities are being scapegoated for factory outbreaks caused by airborne spread
- Epidemiological studies
- A trade union programme
- Doctors in Unite
- References
1. Airborne spread of covid-19
The British Medical Journal published a leading article on 22 August on airborne spread of Covid-19 [1], which summarises what is now very convincing evidence for aerosol transmission through the air. The article says that current official guidance, which says transmission occurs only through contact and droplet spread and that aerosols are produced only during so called “aerosol generating procedures” in hospitals, does not withstand scrutiny, and gets in the way of much needed measures to combat the virus. The authors state, “Heavy breathing, coughing, talking, and singing all generate aerosols……This has important practical implications for infection control, the prevention of outbreaks and superspreading events, and for the new social behaviours that are being implemented in an effort to control the pandemic.”
The article states that airborne spread is now the plausible cause of super-spreader events, and it seems very likely that several outbreaks here in the UK, for example Greencore in Northampton, the garment factories in Leicester, meat and poultry packing plants in Wales and West Yorkshire and Coupar Angus in Scotland have been just such events. It is striking that according to press reports, in some of the outbreaks employers insist they have been fully implementing all recommended workplace safety measures. Greencore is a case in point: the company stated, “All of Greencore’s sites have wide-ranging social-distancing measures, stringent hygiene procedures and regular temperature checking in place”. Yet nearly 300 people working there were still infected.
2. Greencore outbreak
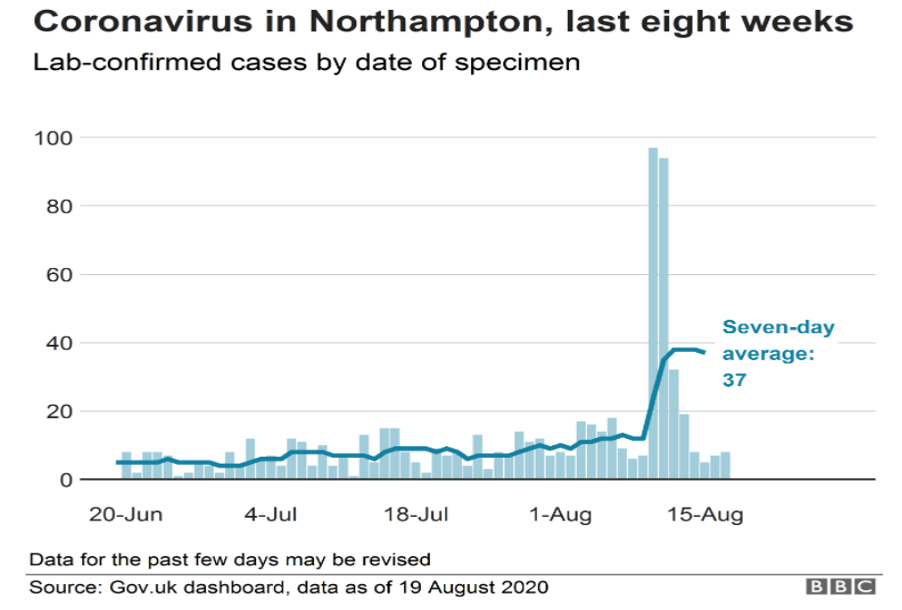
It is instructive to look at the Greencore outbreak in some detail, to ascertain how the virus spread. It is unlikely that a large number workers breached handwashing and distancing measures at the factory all within a few days, especially as management says they are so careful. It is also implausable that community transmission carried infection into the factory to such a large extent. This would mean a large number of discrete, small outbreaks in the community all at the same time, and very many more cases in the community outside the factory, which does not appear to have happened. In fact, the BBC reports [2] that “Testing data and analysis from the Joint Biosecurity Centre shows the spike is “almost solely down” to the outbreak at Moulton Park-based Greencore, which employs 2,100 people”. The timing of the outbreak indicates instead a typical super-spreader event. The graphs below demonstrate this clearly; one is of the Greencore outbreak: there was a low and steady number of cases in the Northampton area until mid-August when there was an abrupt jump in cases – over 200 within 3 days; a typical super-spreader pattern. The second graph is of the super-spreading event in a call centre in Seoul in March 2020, and shows a similar pattern: 94 out of 216 employees working in an open plan office on the same floor became infected over a few days in this outbreak.
Seoul call centre outbreak early March 2020 Source: Park et al, Emerging Infectious Diseases CDC https://wwwnc.cdc.gov/eid/article/26/8/20-1274-f1

We have appended below a press photograph of the Greencore factory floor: assuming this accurately portrays current working conditions, there are lots of people sharing the same, indoor space for many hours at a time each day. We have no information about the ventilation in the factory, but food processing plants are usually kept cool for hygiene reasons, and colder temperatures favour the survival of the SARS-CoV-2 virus. The ventilation often also involves recirculation of colder air in such plants, at least in part, rather than complete air changes with fresh outside air. Even with several air changes per hour it seems that some live virus can still be present in the air indoors (see below). And the direction of ventilation and air flow within the space is also important; it may carry the virus from an infected worker towards others. This is thought to have happened in the well documented restaurant outbreak in Guangzhou. [13]
We do not know if the photograph reflects recent practise, but if so, the lack of mask wearing is striking. Greencore workers told the local press they were “terrified” of being required to work while they awaited test results for Covid-19, and were told it was up to them if they wanted to wear a face mask or not. [14]

3. Tönnies meat packing plant studyIt is helpful to look at a detailed study of a similar super-spreading event also in the food processing industry – at the Tönnies meat packing plant in Germany in June. [3 – not peer reviewed as yet]. The study analysed a range of possible factors involved in the outbreak, including the timing of infection events, spatial relationship between workers in the meat processing plant, climate and ventilation conditions, sharing of living quarters and transport, and performed full viral genome sequences (i.e. genetic fingerprinting) from virus recovered from PCR-confirmed SARS-CoV-2 cases. The viral sequencing established that spread was from a single index case within the factory to other workers, and not from multiple entry points by different workers bringing infection into the plant. It also established that shared accommodation and transport did not play a material role in the outbreak. Over a 3 day period, 29 workers out of 147 who worked the same shift as the index case became infected before the index case was quarantined. 60% of workers within an 8m radius of the index case became infected. In addition, before the workers caught in the first outbreak were quarantined, they had had contact with others elsewhere in the factory, which led to a secondary outbreak leading to over 1500 workers becoming infected in the Tönnies factory overall. This led to a lockdown of a large area in the North Rhine-Westphalia region in western Germany.
3. Tönnies meat packing plant study
It is helpful to look at a detailed study of a similar super-spreading event also in the food processing industry – at the Tönnies meat packing plant in Germany in June. [3 – not peer reviewed as yet]. The study analysed a range of possible factors involved in the outbreak, including the timing of infection events, spatial relationship between workers in the meat processing plant, climate and ventilation conditions, sharing of living quarters and transport, and performed full viral genome sequences (i.e. genetic fingerprinting) from virus recovered from PCR-confirmed SARS-CoV-2 cases. The viral sequencing established that spread was from a single index case within the factory to other workers, and not from multiple entry points by different workers bringing infection into the plant. It also established that shared accommodation and transport did not play a material role in the outbreak. Over a 3 day period, 29 workers out of 147 who worked the same shift as the index case became infected before the index case was quarantined. 60% of workers within an 8m radius of the index case became infected. In addition, before the workers caught in the first outbreak were quarantined, they had had contact with others elsewhere in the factory, which led to a secondary outbreak leading to over 1500 workers becoming infected in the Tönnies factory overall. This led to a lockdown of a large area in the North Rhine-Westphalia region in western Germany.
The diagrams below are reproduced from the study and show: A: the distance between the index case (B1) and spread to other workers; diagram B shows the relationship of distance to infection risk and diagram C shows that spread within the factory was the cause of the outbreak and not shared accommodation or car pools. A full description of these findings is in the paper at reference [3].

It is worth quoting from this study at length:
“Aerosols are believed to be particularly important in cases where a single source transmits the virus toa large number of individuals, so-called super spreading events. Whereas droplets typically travel no farther than 2 m, aerosols can stay in the air for prolonged periods of time and may deliver infectious viral particles substantially beyond 2m distances, especially in indoor settings with low fresh air exchange rates. Factors such as temperature, humidity and air circulation are thought to significantly influence stability and transport of droplets and aerosols and consequently transmission efficiency.
Meat processing plants have recently emerged as hotspots of SARS-CoV-2 around the world. This is thought to result not only from operational practices (e.g. close proximity of workers in the production line combined with physically demanding work that promotes heavy breathing), but also from sharing of housing and transportation that may facilitate viral transmission. The requirement to operate at low temperature in an environment with low air exchange rates is another factor that may promote spread of the virus among workers.
Transmission occurred in a confined area of (the) meat processing plant in which air is constantly recirculated and cooled to 10°C. ……. Analyzing housing and commuting parameters, along with spatial and climate conditions in the work area, this study provides evidence that transmission occurred over a radius of at least 8 meters around the index case…… Physical work and relatively low fresh air exchange rates together with continuous re-circulation of cooled air may have favoured the transmission of SARS-CoV-2…
The universal point of potential contact among all cases was work in the early shift of the beef processing plant. The shift comprises 147 individuals, most of whom work at fixed positions in a conveyor-belt processing line……
….. while some secondary infections may have occurred within apartments, bedrooms or carpools, our collective data strongly suggest that the majority of transmissions occurred within the beef processing facility, with (index) case B1 being at the root of the cluster.
Our findings indicate that a physical distance of 2 meters does not suffice to prevent transmission in environmental conditions such as those studied here; additional measures such as improved ventilation and airflow, installation of filtering devices or use of high-quality face masks are required to reduce the infection risk in these environments.
Our findings suggest that the facilities’ environmental conditions, including low temperature, low air exchange rates, and constant air re-circularization, together with relatively close distance between workers and demanding physical work, created an unfavourable mix of factors promoting efficient aerosol transmission of SARS-CoV-2 particles.
It is very likely that these or similar factors are also responsible for current worldwide ongoing outbreaks in other meat or fish processing facilities. The recurrent emergence of such outbreaks suggests that employees in meat or fish processing facilities need to be frequently and systematically screened to prevent future SARSCoV-2 outbreaks. Furthermore, immediate action needs to be taken to quarantine all workers in a radius around an infected individual that may significantly extend beyond 2m.
In contrast to work-related exposure, shared apartments, bedrooms, or carpools appear not to have played a major role in the initial outbreak described in this study. Nevertheless, later viral transmission within shared living quarters or work rides very well may have been a confounding factor in context of the second, larger outbreak occurring one month after the first outbreak. Our genotyping results are fully compatible with the hypothesis that this second outbreak was seeded by cases related to the initial cluster.
The significance of this study is imminent for the meat and fish processing industry but might well reach beyond these industries, and points to the importance of air quality/flow in confined spaces to prevent future superspreading events
Common operational conditions in industrial meat processing plants promote the risk of SARS-CoV-2 superspreading events. Additional measures such as improved ventilation, optimized airflow management, installation of filtering or ultraviolet light devices or the use of high-quality face masks are required to reduce the infection risk in these environments.”
Community spread and spread among workers outside the factory have been pointed to as the cause of the Greencore outbreak. This seems to be mere supposition rather than any evidence-based assessment for such spread. The Tönnies study involved a similar group of workers, i.e. workers sharing accommodation and transport, and specifically looked at these issues and disproved them as the reason for the outbreak. There is a lack of awareness and therefore no consideration of the role of indoor aerosol spread driving factory outbreaks, which perhaps explains why the press, public and even health experts look for possible explanations outside the factory gates.
4. Preventive measures taken by Tönnies and lessons learned
The study reports that the company took the following measures after the outbreak:
- Hygiene regulations and one-way traffic in hallways were reinforced.
- An internal multi-lingual information campaign was started to raise awareness for all staff of prevention and self-detection of early COVID-19 symptoms.
- Temperature checks were set up to check all employees entering the building.
- Workers were made aware of the availability of testing and were motivated to report any events where they see themselves being at risk. Staff were tested based on self-reported symptoms, possible contacts to other infected persons, returning to work after more than 96 hours absence from work, or possible work place contact with infected colleagues.
- Work place assessments were performed to see if it was possible to extend distances between workers.
- Simple one-layer face masks were made compulsory.
- Regulations to prohibit rotation between working places were imposed. (Shift workers were employed by an outsourcing company who had changed their workplaces according to demand by the employer.)
- Measures in the canteen were imposed to reduce physical contact and to ensure that workers would spend their break times exclusively with workers from their own shift.
- Implementation of the measures was audited within a month by unannounced inspections of the Occupational Health and Safety Experts of the competent authority.
There are a number of important lessons from this study:
- Airborne spread is particularly important in super-spreader events;
- Aerosols can carry virus much further than 2m indoors;
- Temperature, humidity and air circulation (fresh air exchange rates) significantly affect stability and transport of droplets and aerosols and therefore transmission;
- Close proximity of workers on the production line doing physically demanding work and therefore breathing heavily also facilitate transmission. (Other studies have pointed to rapid “line speeds” as an additional contributing factor);
- Early quarantine of possible contacts is essential to limit spread;
- Shared accommodation and transport did not play a significant role in this outbreak; the common factor was working together on the factory floor under these conditions;
- Improved ventilation and airflow, installation of filtering devices, and use of face masks are required to reduce the infection risk in these environments, and in other workplaces which have enclosed indoor spaces.
- Large secondary outbreaks can occur from an initial outbreak in a factory. Press reports indicated an increased number of cases in the surrounding community as well (but this may have been due to increased testing).
- There is a need for surveillance testing in high risk environments like food processing plants, given the large number of super-spreading events which have occurred in them.
- In addition to measures like hygiene, social distancing and temperature monitoring, multi-lingual information campaigns, compulsory face masks and rapid access to testing are important.
- Inspection by regulatory authorities is important to ensure compliance.
While there have also been numerous outbreaks in the hospitality sector, especially linked to pubs, the workplace appears to have now become the frontline in the battle against Covid-19, both here and across the EU. [4] [5]
5. Growing evidence and consensus around aerosol spread
Aerosol scientists, mainly in the US but also in Australia and elsewhere, and here in the UK (e.g. Professor Catherine Noakes at the University of Leeds, who sits on SAGE), have been convinced for some time that aerosol spread is a major route of transmission. In July, 239 scientists wrote to the World Health Organisation (WHO) asking it to recognise airborne spread and amend its guidance. WHO did shift its previous rejection of the idea and said aerosol spread “cannot be ruled out”. Since then there has been further evidence, including the successful culturing of live virus from the air up to 4.8m from infected patients in hospital rooms. (A surprising and concerning finding was that the rooms had fairly good ventilation rates as well as UV light air sterilisation, but live virus was still able to be cultured from the air.) [6]
Meanwhile official documents from SAGE have referred to aerosol transmission on a number of occasions, [7] [8] and some professional associations’ guidelines now include advice on the risks of aerosol spread; for example, the Primary Care Respiratory Society says that routine assessments of patients by means of spirometry should be avoided due to the risk of droplet and aerosol spread. [9]
Aerosol spread is officially recognised in Germany and Japan and recently the French employment minister, Elisabeth Borne, stated that compulsory mask wearing from 31 August in France, “reflects a growing scientific consensus that the virus is transmitted not only in big drops projected when a person coughs or sneezes, but also in smaller ones suspended in the air breathed out by infected people that accumulates in enclosed spaces”. [10]. Nicola Sturgeon spoke of the risk of aerosol spread in schools in Scotland on 24 August, stating her government was considering face coverings for secondary school students in communal areas. [11]
In the US a number of institutions are actively looking at ventilation requirements in indoor spaces, using CO2 monitors as a proxy measure for adequacy of ventilation, and the addition of portable air filters to make indoor spaces safer, including in schools and universities. A clear and practical article on this from the University of Colorado is at reference [12].
6. Workers and local communities are being scapegoated for factory outbreaks caused by airborne spread
We have seen in Leicester and other areas of the Midlands, accusations that outbreaks in factories have been due to workers and/or local communities failing to observe social distancing measures. There has been racist scapegoating of Asian communities, blaming them for local spikes in infection caused by factory outbreaks (in the Leicester garment factories for example), which very likely have involved airborne transmission. We have seen a social media post about the Greencore workers saying, “I don’t feel bad for most of the staff. The Eastern Europeans never followed regulations like distancing and not mixing in large groups in lockdown in March onwards. They don’t care.” The role of airborne spread needs to be understood, and communicated to all concerned during these outbreaks. Ignorance of how Covid-19 spreads is leading to victim-blaming of people who become infected, when attention should be directed to employers, public health officials and government for solutions.
It is notable that in many of these large outbreaks, workers are poorly paid and are on insecure short-term contracts. Many receive only Statutory Sick Pay; as a result they have had to rely on food banks, and some have lost their homes as they could not afford to pay rent. All workers forced to take time off due to having Covid-19 or having been a close contact of an infected person should receive full pay while isolating. Not doing so is inhumane, and is obviously also self-defeating, as some workers will go to work like those who were made to do so at Greencore while awaiting test results, and thereby compromise efforts to curtail the outbreaks. The government’s recent derisory offer of £13 per day for workers having to isolate is clearly wholly inadequate. It has been described as “a slap in the face” by a Council leader, and also only applies to areas with already high infection rates. This is clearly wrong, we want to prevent infection rates going up, not reacting when they have already become high. A proactive, preventive approach is needed.
7. Epidemiological studies
We believe it would be also be very helpful if detailed epidemiological studies, like the one done in the Tonnes meat packing plant, could be conducted in future outbreaks here in the UK, to better understand and learn from them. Hopefully some are being done but we have yet to see any of these.
8. A trade union programme
- Employers must recognise airborne spread as a covid-19 risk and take action to assess and minimise risk.
- Improved ventilation and airflow, installation of filtering devices, and use of face masks are required to reduce the infection risk in these environments, alongside other safety measures against Covid-19.
- Trade union supervision and control of workplace safety.
- Weekly surveillance testing on site of all workers, including management, in addition to easily accessible testing for anyone with symptoms or in contact with Covid-19.
- All workers forced to take time off due to having Covid-19 or having been in contact with it should receive full pay while isolating. No-one should have to work while awaiting test results for symptomatic or contact testing.
9. Doctors in Unite
We are a national doctors’ trade union within Unite the Union; our members include working and retired GPs and hospital doctors and dentists from a range of specialties, as well as public health doctors and non-medical public health specialists, from across the four nations of the UK. We are party to the BMA negotiating machinery by virtue of an agreement with the BMA dating from 1950 and are the only medical trade union recognised in local government. We have been involved throughout the pandemic, both in our day jobs, and also raising issues around PPE, “Covid-safe” workplaces and campaigning on the critically important requirement for locally based ‘Find, Test, Trace, Isolate and Support’ services run by the DPH in each borough.
We will also continue to lobby for a change to official guidance around transmission of Covid-19, although with the abrupt axing of PHE this may be difficult.
10. References
[1] https://www.bmj.com/content/370/bmj.m3206
[2] https://www.bbc.co.uk/news/uk-england-northamptonshire-53860426
[3] https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3654517.
[6] https://www.medrxiv.org/content/10.1101/2020.08.03.20167395v1
[13] https://wwwnc.cdc.gov/eid/article/26/7/20-0764_article#tnF1